Health policy
The whole is less than the sum of its parts
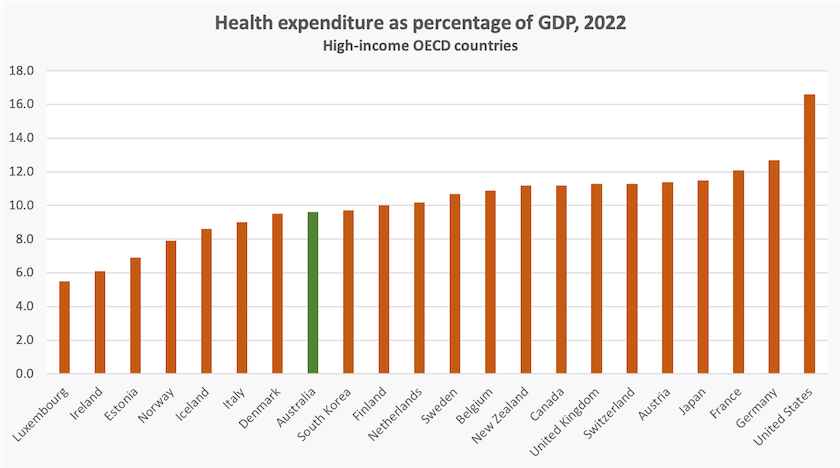
In comparison with other high-income “developed” countries, Australia does well in achieving value-for-money in health care.
We shouldn’t congratulate ourselves, however. Because our population is younger than that of other prosperous countries, we shouldn’t have to spend too much on health.
Our health outcomes are good, but maybe we could do even better, or extend publicly-funded health care to more people, if we could use our health care more efficiently. Three recent articles provide examples of how that could be achieved.
Economies in buildings
Martyn Goddard challenges policymakers to think of improving outcomes without spending any more money in his post Want to save public hospitals? First, stop being stupid. “Under-funding is not the main reason for the crisis in Australia’s public hospitals”, he writes. “A far bigger problem is systemic stupidity”. His focus is on the way governments handle capital funding for health care.
He is not blaming hospital administrators or clinical staff for stupidity. The shortcomings he identifies are the systems within which they operate, subject to the decisions of ministers and senior public servants.
He identifies building cost blowouts as one source of wasted expenditure. When it comes to hospitals, he writes, “the standard government plan is to build first and consult later. So, too often, critical faults aren’t identified until the building is well under way – or, in some cases, already finished”. Decisions to build hospitals and where to locate them are not subject to the same rigorous benefit-cost analysis that applies to transport projects, for example, and the processes of specifying, tendering and supervising hospital capital works are not always competently handled. (Yet another manifestation of the loss of skills in our public services.)
The other major waste is in the misallocation of resources – “beds” – between acute-care public hospitals and nursing homes. Too many expensive hospital beds are occupied by people whose needs would be at least as well served – perhaps better served – in nursing homes. But we haven’t built enough of them. Goddard writes: “In Australia, it costs around $1,400 a day to keep someone in an acute hospital bed without doing anything for them apart from basic nursing. In contrast, the Productivity Commission calculates that the patient-day cost of residential aged care is $243 a day”.
Better use of information technology
From another angle the Productivity Commission considers the opportunities for administrative saving, and better directed care, if the health care sector were to make better use of information and communication technologies. Its research paper Leveraging digital technology in health care covers four areas where the sector could make better use of existing and developing technologies—electronic health records, telehealth, remote care, and artificial intelligence.
In some cases, particularly in telehealth, there are regulatory impediments to improving use of information technology. But most problems lie in the fragmentation and non-standardization of systems. Although hospitals are some of the last places, other than museums, where one can still see fax machines in use, most establishments have developed their own systems, including electronic health records. The researchers note, in relation to these records, that they are generally compiled and stored as PDFs, rather than as relational databases, in which information can be standardized and interrogated in different ways depending on users’ needs. The problem lies in the fragmentation of our health care arrangements themselves, with different levels of governance (Commonwealth, state, district hospital boards, private operators) and different channels of accountability. In short, the digital sub-systems cannot talk to one another and are unfriendly to users.
Fraud and waste
A recent edition of the ABC’s Four Corners – Worse off after surgery: Exposing Australia’s profitable pain industry – reports on an investigation by Adele Ferguson into the way some medical practitioners have exploited patients, Medicare, and private health insurers through over-servicing and by billing for services that were never provided. (The TV program, linked above, is supplemented with an informative website, The price of pain.)
This is a specific example of a problem built into our health care arrangements, as what may be called an ideologically-driven design fault. That is the use of private insurance as a major part of our health care arrangements. It’s not that private insurers themselves are guilty of fraud or over-servicing. It is not in their interest to be billed for unnecessary or undelivered services, and as the Four Corners program demonstrates, the private insurers were no less concerned about fraud and waste than the investigative journalists.
Rather, the problem lies in the inability of a fragmented private insurance industry to control service providers’ use or prices. Insurers refer to this problem by the quaint name “moral hazard”. People reasonably choose to pool their risks through health insurance. But insurance of any type, private or public, suppresses the price signals that ration usage in markets. There’s no difference in the logic “Medicare will pay for it” and “Medibank/NIB/HCF will pay for it”.
Effective control of moral hazard can be exercised only through a single national insurer, almost always government-owned and taxpayer-funded. That point is most clearly illustrated in the graph at the beginning of this post. The USA is the standout example of the cost of private insurance, which has resulted in that country having the highest-cost system, poorest accessibility, and some of the worst outcomes for the population.
Private health insurance is essentially a “privatized tax”, which does what the ATO and Medicare do, but with much higher administrative costs and much less capacity to control moral hazard. You can find a short explanation of this in a Conversation contribution: Health funding: something else for Turnbull to worry about, and in a fully-referenced 2016 paper Private Health Insurance and Public Policy.
The budget and health
Peter Breadon and Anika Stobart of the Grattan institute have a Conversation contribution: Cheaper medicines and a new approach for mental health care. Will the budget make us healthier?
It’s a generally positive evaluation of the government’s policies, including an improved approach to mental illness, investment in more urgent care clinics, and some other specific measures. But there is no sign of the promised centre for disease control and funding for dental care once again misses out.
Martyn Goddard’s evaluation on his Policy Post – The budget that forgot health – is less positive. The governemnt is making much of its extra 29 urgent clare clinics. They’re useful, but that increment won’t make a dent in the workload of public hospitals. He points to evidence that medical services are underfunded and underresourced. Two years ago 90 percent of GP fees were covered by Medicare: now only 84 percent of fees are covered. More woringly the rate of GP attendances per 1000 population has fallen from 678 in May 2022 to 500 in March 2024.
Underfunding can be attributed to the government’'s general reluctance to riase taxes and increase publc expenditure. Underresourcing relates to a shortage of GPs, stemming from a long period of underfunding universities, mainly on the Coalition’s watch: there is little the government can do about this in the short term. The Coalition’s proposal to cut immigration, including skilled immigration, would make the situation far worse.
Covid-19 is still around
Remember that pandemic? Remember isolation, travel restrictions, masks, a RAT test every time you felt a little unwell?
Well Covid-19 hasn’t gone away, and is still resulting in avoidable deaths. Hospitals provide ideal incubation conditions for Covid: about 9 percent of people who catch Covid in hospitals die after contracting the virus. To quote figures from the ABC’s Hayley Gleeson’s post, Hundreds of patients died after catching COVID in Victorian hospitals, new data shows. “[Nationally] at least 6,212 patients caught COVID in hospital in 24 months – 3,890 in 2022 and 2,322 in 2023. Of those, 586 died – almost six per week, on average – with men dying at a higher rate than women. (cf. homicides ~ 380. road fatalities ~ 1270.)
Gleeson goes on to illustrate the effectiveness of RAT tests and use of N95 masks in hospitals, which save lives and money. But understandably, mask fatigue has set in.