Health care
Our primary health care system needs repair
The pandemic has heightened our awareness of stress on our health care system. Stress on hospitals is abating somewhat, but it is still high, as confirmed by accounts of overcrowded emergency departments. And there is no letup in the stress on GP services which was worsening even before the pandemic hit. It has been getting harder for people to make a timely appointment, co-payments are increasing, and in some non-metropolitan regions GP practices have closed.
The consequences are serious: some people are missing out on early diagnosis of conditions that will develop into serious illness if untreated, people with limited means are finding GP services unaffordable, hospital emergency departments have become even more overcrowded. A combination of these factors is worsening the incidence of disease, increasing the cost of treating disease, and is widening inequities in health care.
The Grattan Institute has put the case for a fundamental reform of the way we organize and fund GP services: A new Medicare: strengthening general practice. It states that “a system designed for an earlier era hasn’t been updated to respond to the rise of chronic disease, or to tackle gaping disparities in access to care, rates of disease, and life expectancy”. We need a new Medicare, with three big changes.
The first change is to break from the model where the GP is responsible for all on-site services. GP practices should include other clinicians, such as nurses and physiotherapists, but such integration is not encouraged by current funding models. We are under-using the skills of these clinicians while over-working GPs.
The second is to reform funding to allow GPs to spend more time on complex cases. “The current model is broken, actively discouraging team care and rewarding speed, not need”.
The third is a more general recommendation about directing attention to the performance of GP services in terms of outcomes, with appropriate indicators of how well the system is working, rather than the present focus on throughput at least possible cost to the health budget.
The report is rich in data, describing a system with slowly worsening stress, rather than any immediate crisis. It provides hard data on the growing burden of mental health conditions on GP practices, and the way the most disadvantaged have most need of health services, but these are the people whose needs are most often unmet.
The report is about reform within the principle of Medicare as a universal system: it does not recommend a departure from that model (for example, by allowing private health insurance to fund GP services).
No, Covid-19 hasn’t gone away
It was inconvenient for the prime minister to be hit with Covid-19 just before crucial negotiations on energy pricing, but at least it reminds us that this wave is real, and hearing his pained voice from Kirribilli House suggests that even though he is well-vaccinated and has been struck before, the second dose isn’t much fun either.
Covid-19 is still a killer. In November 475 Australians died of, or with Covid, up a little on October.
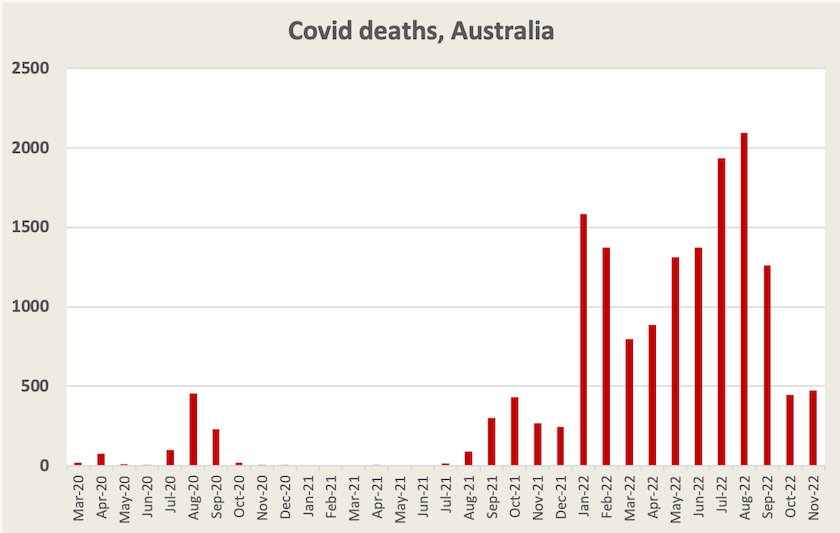
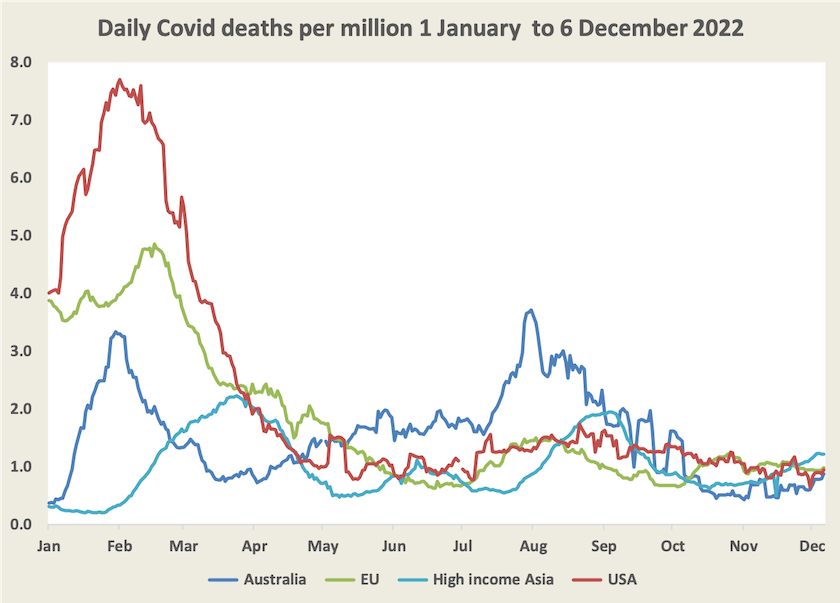
Deaths have still been rising into December, as they have been in other high-income Asian countries. At around 0.9 daily deaths per million population, this wave is still serious, but less deadly than earlier waves this year.
Writing in The Saturday Paper John Hewson urges us to take this wave seriously: We need Covid-19 mandates. He acknowledges the political difficulties for governments in re-introducing mandates, particularly at this time of the year, but he is critical of the way governments have progressively relaxed mask mandates and isolation requirements.
Pulling together the views of public health experts, he writes that “in the absence of sensible and effective health measures – such as mandatory masks in most public spaces and on public transport, and isolation for infectious people – persistent waves of infections next year and beyond will almost certainly result in an ever-increasing social and economic burden on Australian society”. He also calls for attention to ventilation in public spaces and workplaces.
Along the way he has some words about Scott Morrison’s “self-absorbed, delusional behaviour” in the politicized way he handled the pandemic, which led to our switch from having one of the world’s best approaches to Covid-19 in 2020 and 2021 to one of the worst in 2022.
Hewson could also have mentioned our state governments’ lackadaisical approach to reporting Covid-19 data, which has been so sloppy that the noise of revisions and lumpy reporting of several days or weeks of cases and deaths has obscured information about trends. The situation became worse in September when they switched from daily to weekly reporting, just as this wave was starting to break out. That means data on hospitalizations and deaths, as provided by the ABC on its Covid-19 site, has a significant lag. Pulling together scraps of data The Guardian’s Caitlin Cassidy notes that cases are probably still rising, but that they could peak before Christmas.
Compared with the measures we accepted during the early days of the pandemic, the measures Hewson calls for should be easy to comply with. And they can be remarkably effective in reducing the virus’s spread. The mathematics of reproduction are such that small interventions can have large system-wide effects. That’s the mathematics applying to threatened species, compound interest, rabbit populations and many other phenomena. We need to understand that Covid-19 and other infectious diseases are governed by the same mathematics.