The pandemic and other health policy

The pandemic, cases down, but hospitalizations and deaths are still high
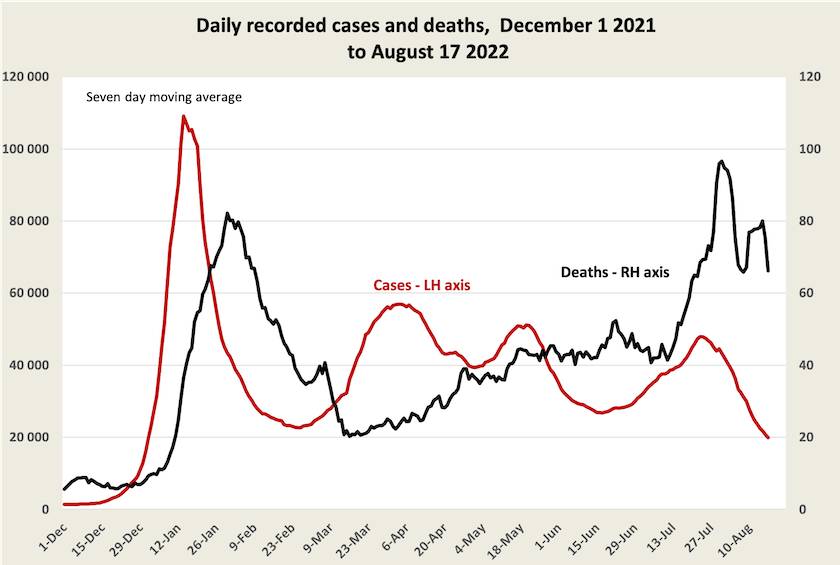
Recorded cases continue to fall. Because people are probably slackening off in their reporting of cases, not too much trust should be placed in the absolute numbers, but the trend is encouraging.
Unlike case numbers, figures on deaths are generally accurate, but some state authorities allow them to accumulate before reporting, and there is no method of statistical smoothing that can present a clear trend from such scatty data. That’s why the graph looks so bumpy: the double peak may simply be an artefact of lumpy reporting..
At around three daily deaths per million population, our incidence of deaths is still about twice that of the EU, and most other “developed” countries. It is notable that New Zealand also has a similarly high daily death rate. Because we are now about three weeks past the caseload peak, deaths are probably falling, but it will take a few more days of data to confirm the trend.
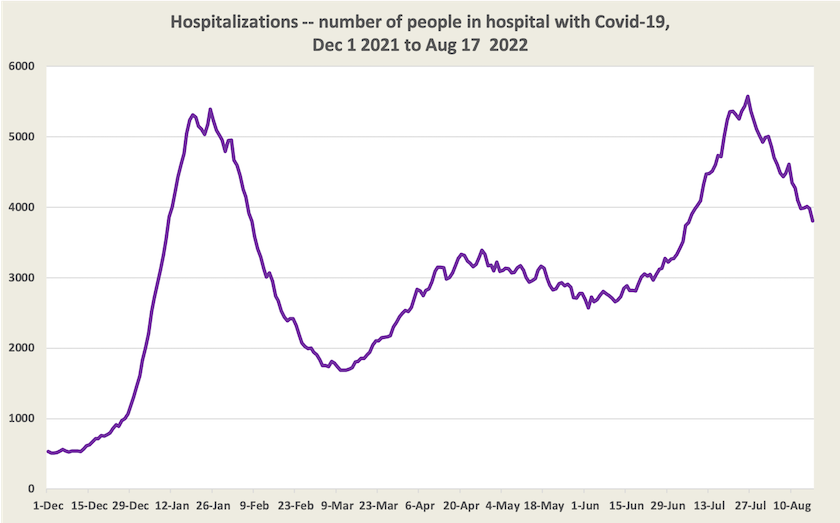
Hospitalizations are falling, but are still high. As yet there would be little relief on our overworked hospitals.
In the race between vaccine development and the virus’s capacity to mutate, a Moderna vaccine that provides strong (not absolute) protection against the original strain and the first BA.1 Omicron variant has been approved by one European country, and other countries are likely to follow. Early data suggests it gives better protection against other sub-variants of Omicron than the vaccines we have been using to date.
Medicare: in need of booster shots
Medicare, our (nominally) universal health care system is struggling. Our hospitals are crowded, and it is getting harder for people to find a medical practitioner who uses direct billing (commonly known as “bulk billing”) without charging the patient. In many situations, particularly non-metropolitan regions, it is hard for people to find a medical practitioner at all.
Higher rebates for GP visits may help solve the problem of falling rates of direct billing, but it would take a long time for any injection of funds to increase the supply of GPs.
These problems are addressed in an article in The Guardian – Australians think they have universal healthcare: that’s no longer true – by Jennifer Doggett.
Mark Sawyer, of Michael West Media summarises the problems with the Medicare rebate for standard GP consultations. It was frozen by the Coalition for six years, and this year it is indexed at a mere 1.6 percent, paying $39 for a 20-minute consultation. (Try finding a plumber or electrician with those rates.)
The government is talking about its $750 million “Strengthening Medicare Fund”, but that’s a drop in the ocean of the Commonwealth’s $106 billion health expenditure.
A dispute has arisen over the actual rates of direct billing, outlined in a Guardian article by Melissa Davey and Stephanie Convery: “Not honest”: new health minister dismisses Coalition election claim that bulk billing had hit 88%, and the subject of a 7-minute interview with Health Minister Mark Butler on the ABC’s PM.
The previous government’s claim that 88 percent of GP services are “bulk billed” doesn’t align with people’s experiences, and data from the Institute of Health and Welfare shows that a third of people are paying gap fees. The average gap fee is now around equal to the Medicare rebate. The explanation is that many consultations involve more than one Medicare item, and while some of these items may be direct-billed, others are not: the 88 percent refers to the percentage of items, not the percentage of consultations.
Butler’s interview gives a clear explanation of the numbers, but anyone expecting him to defend Medicare as a universal scheme, free at the point of delivery, will be disappointed. He seems to see direct-billing as a measure of distributive welfare or charity, rather than as a program of social solidarity.