The pandemic and other health policy

Perhaps this wave of Covid-19 really has peaked in Australia
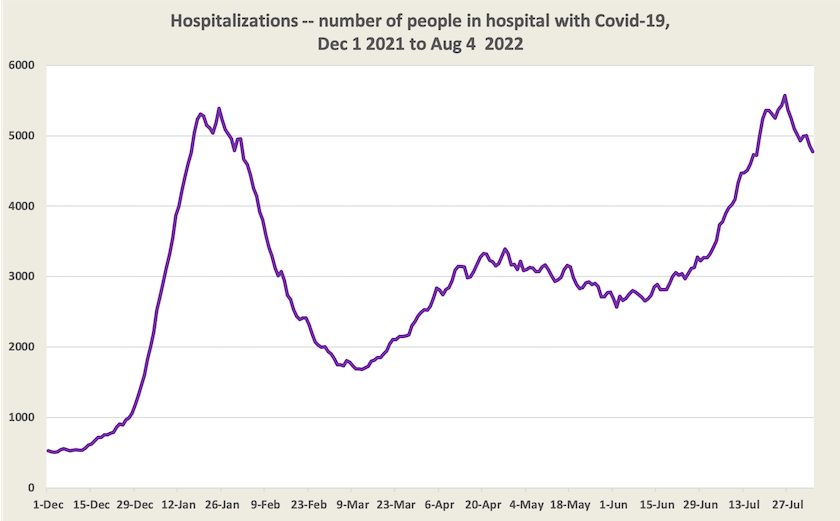
There are encouraging signs that this wave of Covid-19 and other dangerous respiratory infections may have peaked in Australia, according to epidemiologists. Covid-19 hospitalizations reached their maximum almost two weeks ago. Case numbers seem to have reached a high in most states a few days earlier, but besides the usual bias toward under-reporting cases, figures have been distorted by a huge backlog of cases having been recorded in Queensland. Data for deaths is similarly ambiguous, because Victoria recorded more than 100 deaths in one day, as a result of a backlog in reporting deaths.
I’m therefore dispensing with the graph on cases and deaths this week, because it’s too much influenced by these large figures that may refer to deaths and cases that happened many weeks ago.
Normally laxity in recording cases and deaths is not a serious matter. But it confirms the opinion of public health experts that governments and the public are starting to treat Covid-19 as yesterday’s news, even though it’s still raging in the community, overloading hospitals and killing people, and that we are becoming careless about reporting cases.
Angelica Silva of the ABC’s digital journalism group warns that we have become too reliant on RAT tests, even though their false negative rate is high (they are far less likely to give false positives), and that Australia is behind in taking up testing technology for coronaviruses and influenza. If we are progressively relying more on RATs than PCRs, and if new variants are less well detected on RAT tests, then our under-reporting of cases is getting worse.
In an article by the ABC’s Andrew Thorpe – Australia's public health messaging isn't hitting home like it used to. Here's why – epidemiologist Amalie Dyda suggests that governments haven’t been very good at explaining their advice to people. As the disease takes new turns our behavioural response should change, but governments haven’t explained why. Stephen Duckett notes the problem of the politicization of Covid in the pre-election period. “Labor wouldn't talk about it, because the second they used the C word the Murdoch media would jump on them as 'the party of lockdowns'”. (For confirmation of the politicization of Covid, next time you see a TV clip from the House of Representatives, look at the distribution of masks either side of the House.)
With 100 Australians dying daily of Covid-19, Australia has one of the highest death rates of all “developed” countries. That’s around 3.8 deaths per day per million population, compared with 1.5 per million in the EU. In high-income Asian countries, deaths per million are even lower – Singapore 1.0, Japan 0.9, Korea 0.5, Malaysia 0.4. The ABC’s Emily Clark notes mask-wearing in Asian countries is helping to keep deaths rates low. Masks are compulsory in some countries, but even in countries where masks are not mandated, such as Japan, mask-wearing rates are high. It’s about people seeing public health as a matter of social obligation.
Public health – don’t forget the engineers
Campaigns on Covid-19 are mainly about individual behaviour – social distancing, wearing masks, and getting vaccinated. All are effective in suppressing the spread of Covid-19, but it’s easy to overlook ventilation.

Open windows, a high-tech public health innovation
On the ABC’s Health Report – Do we need another healthcare revolution – Tegan Taylor starts with the classic public health story of John Snow and the Broad Street pump in the nineteenth century. (If you’re not familiar with the story it’s worth a listen, for it stresses the contribution engineers, in providing clean water and sewerage, have made to our health and increased life-expectancy.)
The engineering story of our time is ventilation. There is a close relation between the stuffiness of an indoor space and the transmissibility of air-borne diseases, such as Covid-19. We can get a subjective impression of stuffiness by catching an elevator in a large building. A more objective indicator of air exchange is given by the concentration of carbon dioxide, which can easily be measured with a carbon dioxide monitor. Taylor took a monitor around different spaces – a car (high), a commercial airplane in flight (very high), and a meeting room (high). In some situations we can control ventilation (open a window) or avoid stuffy places (use the stairs rather than the elevator), but in other situations it’s about engineering design, such as building heat-recovery ventilation into buildings, a way to keep a supply of fresh air without losing heat.
Health policy stalled
Some older Australians can remember how in 1974 the Whitlam government risked a double-dissolution election to establish Medibank, the forerunner of Medicare, and how the Hawke government in 1983 made the re-establishment of universal health care – Medicare this time – a priority.
In later years however, governments have lost enthusiasm for reform. As problems have arisen there have been work-arounds guided by fiscal constraints rather than sound economics, compromises that have yielded to interest groups (particularly health insurers and pharmacists), and deals between the Commonwealth and states for funding hospitals. There remain gaps in important areas of care, particularly dental care. There are long-standing demarcation disputes between health professionals, incentives for cost-shifting between governments, a lack of integration between primary care and hospital care, a neglect of funding for public health, and all of this is in a sector that has been extraordinarily conservative in taking up productivity improvements enabled by information technology: Australian hospitals are some of the last places where you can see fax machines still in use.
Martyn Goddard’s Policy Post takes us into the health policy landscape: The loneliness of the long-distance health reformer: Stephen Duckett on politics, bureaucracies and the pandemic. It’s about the policy processes, rather than the policies themselves, that have brought us to this point where every part of our health care arrangements is overworked and fundamental reform is not on the agenda.
It’s partly about the way the inertia of a large organization like the Commonwealth Health Department works against fundamental reform. Incremental reform is the default mode, and long-standing problems tend to be seen as immutable aspects of the landscape. It takes the objectivity of an outsider to see the need and opportunity for fundamental reform. Also, there has been a dearth of policy skills in the Department. In fact, during the Coalition administration, health policy was handled by the minister and a small cadre of political advisers, who had no inclination to listen to the Department for policy advice.