The pandemic – no, Scott, it is still raging
The SARS-CoV-2 virus is most inconsiderate in the way it has timed its latest outbreak to overlap with our election campaign. Cases are rising strongly and deaths are not far behind.
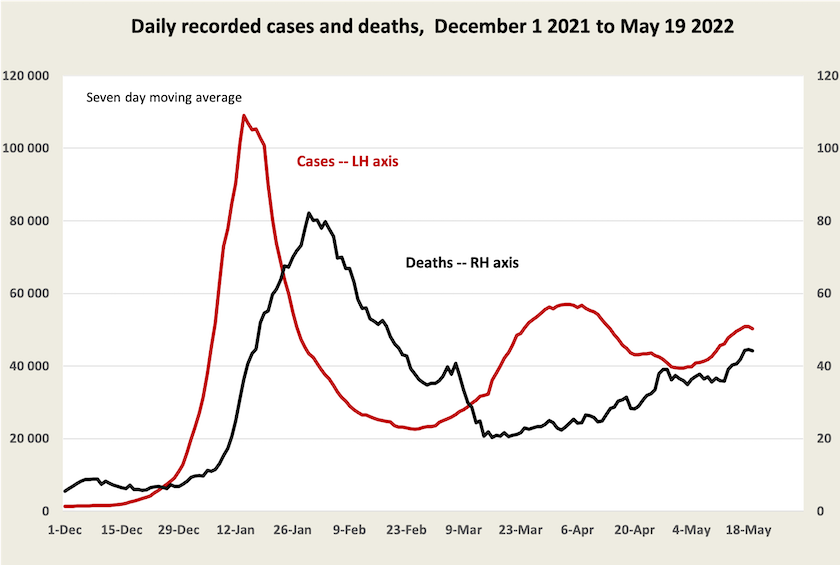
Over 2020 and 2021, thanks to strong action by state governments, there were only 1000 deaths of people with coronavirus in each of those two years, but this year so far there have been 6000 deaths of people with Covid-19[1]. At our present rate of deaths, 44 a day, there would be 16 000 deaths over a full 12-month period.
As a basis for comparison, every year 140 000 Australians die from all causes. We cannot simply add 16 000 to that number and claim to represent the additional consequence of Covid-19 however. Many of those dying with Covid-19 are not necessarily dying from Covid-19. Covid-19 deaths are concentrated among people with a high rate of deaths from all causes. About 60 percent of people diagnosed as having Covid-19 at time of death are aged 80 or older, for example.[2] About a quarter of the deaths so far this year have been of people in aged care.[3] To make the situation harder to interpret this outbreak coincides with the influenza season, and after a two-year lull (assumingly a by-product of masking and social distancing associated with Covid-19), influenza has returned in significant numbers.
It will be some time before there is an estimate of excess deaths resulting from Covid-19. Only then will we be able to start to estimate its full effects, including severe cases of Covid-19 having overloaded hospitals and therefore denied care to others.[4] Then there will be a need to examine the consequences apart from deaths, including the effects of “long covid”, and the economic effects of absences associated with Covid-19.
Although these figures will not be available for a long time, there is plenty of evidence that Covid-19 is a serious and present problem. Rising case and death numbers cannot be ignored. Nor can reports of unplanned absences affecting many services. And in some states, particularly Western Australia where the Omicron wave was delayed, and Victoria, where cases and deaths are rising strongly, there is hospital overcrowding, deferral of elective procedures, and high stress on already heavily overworked health care workers. If Covid-19 deaths are simply displacing other deaths, we would not expect to see such a surge of pressure on public hospitals.
On ABC’s Breakfast program Sharon Lewin of the Doherty Institute explains the situation in an 11-minute interview: Should we be worried about high Covid case numbers? Covid-19 is here to stay, and it will wax and wane in its intensity. In response we will have to be ready to do things to slow its spread, such as wearing masks in crowded indoor spaces. She warns that the present outbreak is serious, particularly in terms of the pressure it is putting on hospitals. Deaths are high and rising because cases have been rising, but in comparison with earlier waves of Covid-19 the rate of death per case is much lower.
In fact the death rate per case is around 0.12 percent, or one in every 860 cases recorded. That reflects a rise over the last few weeks: in early April it was around 0.06 percent, or one in every 1730 cases. Most of that rise has been in Victoria, where it is now 0.18 percent, or one in every 560 cases.[5] Maybe these figures overstate the extent to which the death rate is rising, if more people are not bothering to report positive tests or Covid-19 symptoms. Or maybe they reflect waning vaccination protection, or failures of at-risk sufferers of Covid-19 to obtain and use anti-viral medication.
Rising case numbers, rising deaths, and hospital crowding haven’t stopped Morrison, however, from asserting that the pandemic has now passed and from stressing the influence of co-morbidity – people with Covid-19 dying from other causes.
He seeks to claim credit for our nation’s overall low number of Covid-19 deaths, ignoring the benefit of geography, and ignoring his own indifference to Covid-19 – his inclination to “go to the footy” rather than to deal with Covid-19 when it first arrived, his “not a race” attitude to vaccination, and the pressure he put on states to “open up”, even when the more deadly Delta strain was raging among a relatively unvaccinated population.
Compared with other countries Australia could be doing much better. While we did reasonably (but not outstandingly) well with achieving a high two-dose vaccination level, our performance on a third dose has been pathetic. Only 53 percent of Australians, or 66 percent of our adult (16+) population has had a third dose, and vaccination rates have almost stalled. Our 53 percent compares with 74 percent in Singapore, 72 percent in South Korea, and levels in the 60 to 70 percent range in most high-income European countries.[6] Within Australia there are huge variations state-by-state: the ACT has a 62 percent third-dose vaccination level, while at the other end of the scale Queensland’s third-dose vaccination level is a miserable 45 percent, and it’s even lower in regions away from the Brisbane conurbation.[7] In Victoria, where cases and death rates are particularly high, experts are noting waning immunity as time passes since people had their second dose.
A prime minister who cared about the well-being of Australians would be urging us to get those vaccination levels up, rather than adding to a sense of complacency. But people’s wellbeing is only of secondary importance to Morrison. He wants to keep the anti-vaccination movement onside, with the hope of gaining preferences from the UAP, and he wants to run a scare campaign about Albanese re-introducing tough public-health measures, such as mask mandates.
1. These are rounded figures from Juliette O’Brien and her colleagues on the website Covid-19 in Australia. They align closely with WHO data. The precise figures are 909 deaths in 2020, 1432 in 2021, and 5721 up to 19 May 2022. ↩
2. These are NSW figures, from their weekly surveillance report, in the week ending 14 May. ↩
3. Commonwealth Covid-19 outbreaks in Australian residential aged care facilities. ↩
4. The ABS has had a go at measuring excess deaths in Australia, with findings in a publication Measuring Australia's excess mortality during the COVID-19 pandemic. That takes us up to the end of 2021, and unsurprisingly there is hardly any evidence of excess deaths in 2020 or 2021. The figures for 2022 are likely to be quite significant, however, if other countries’ estimates are any guide. ↩
5. These figures are based on data from Covid-19 in Australia (see footnote 1), based on a calculation of deaths divided by cases three weeks earlier, all smoothed over 7 days. ↩
6. Our world in Data covers almost all countries. ↩
7. The ABC vaccination tracker. ↩