The pandemic
World
Worldwide cases and deaths continue to decline – at least for those countries that report cases and deaths to the WHO.[1]
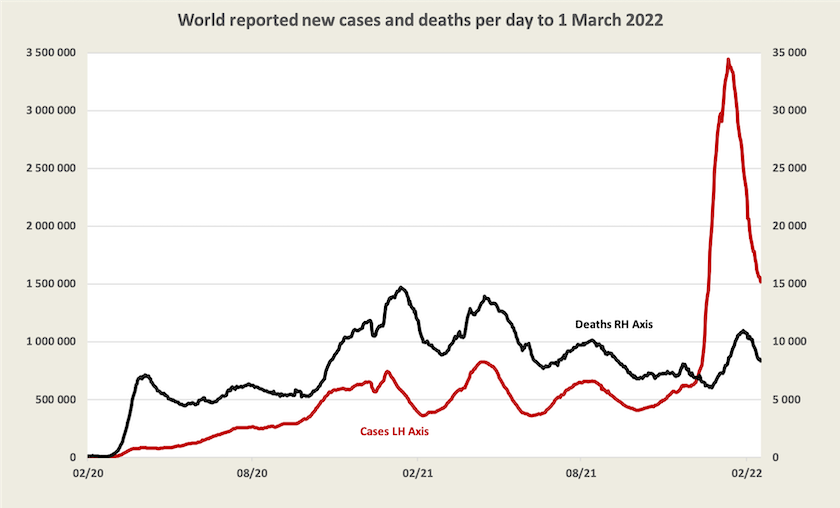
Although worldwide recorded deaths are falling (by 13 percent over the last week), in some countries with high vaccination rates and strong public health measures they are rising. Britain’s John Campbell, in one of his long podcasts (24 minutes this time), drawing on reliable data sets, explains that many people are dying withOmicron, not necessarily from Omicron. He presents strong evidence confirming that Omicron has a low death rate. International comparisons are difficult because different countries have different ways of recording cause of death. He also has some observations on long Covid: it seems to be most prevalent among people in their middle age.
Worldwide there are only four months left for world vaccination levels to reach 70 percent by mid-year. At the present rate that will not be met.
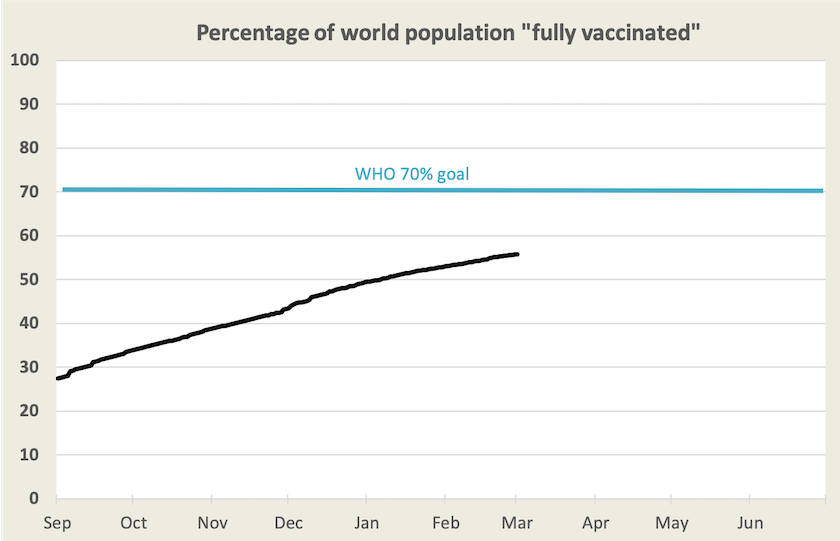
Only a few countries, including western Europe, China, Japan, Canada, most of South America and Australia have met or exceeded that 70 percent goal. India, Mexico, most southeast Asian countries and a few other countries are on track to meet it. But almost all of Africa, the USA, Russia and many middle-eastern countries are not on track. The problem lies not only in supply, but also in countries’ capacity to distribute and administer vaccines. In our region Papua New Guinea, with only 3 percent of the population vaccinated, is an example of such a country.
1.Even if deaths are reasonably accurately recorded (in some countries deaths are fudged for political reasons) case numbers are generally understated because of under-reporting, under-testing and the presence of asymptomatic cases.↩
Australia
Cases
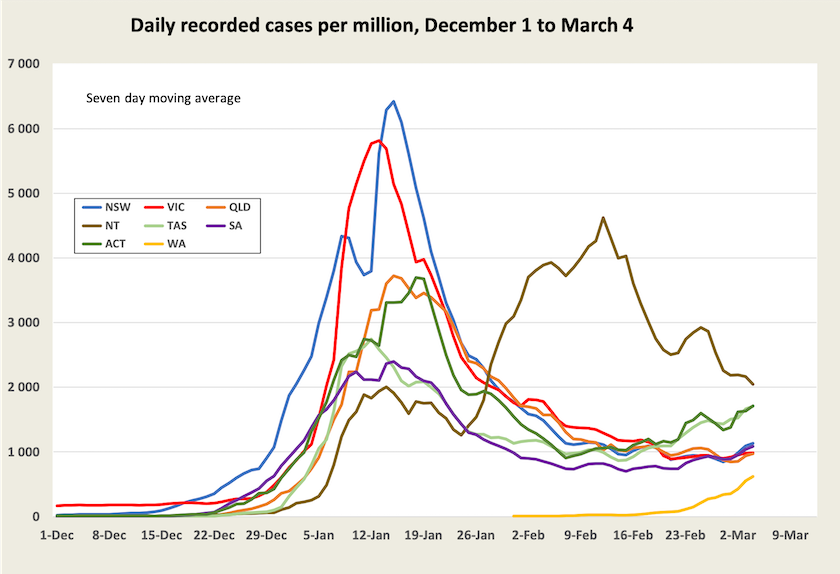
New recorded cases are now running at about 22 000 a day and are rising. That rise could have several different explanations: the loosening of restrictions, waning vaccine immunity, the more infectious BA.2 sub-variant, and more reporting because rapid antigen tests are more available. The state breakdown of recorded cases is shown below.
Note that cases in Western Australia are now in a stage of strong exponential growth, but as Norman Swan explains on Coronacast, Western Australia, in staying isolated while earlier waves passed and as vaccines were developed and distributed, has put itself in a good position compared with eastern states.
Hospitalization
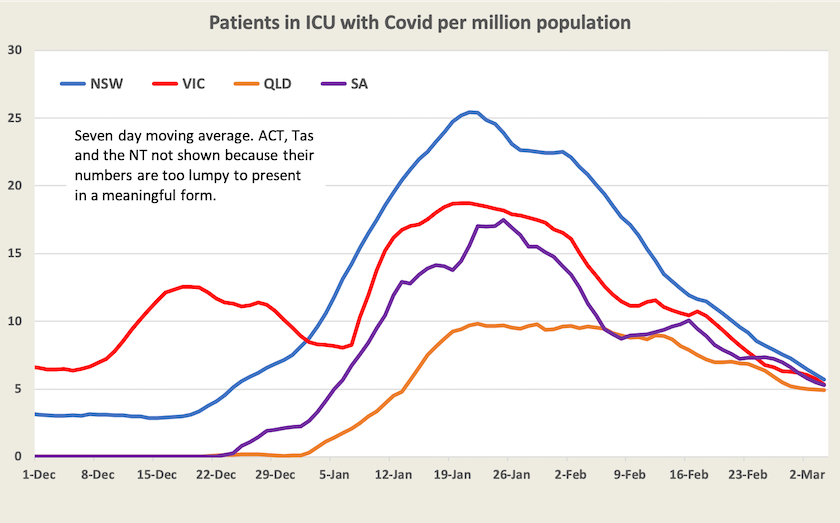
Hospitalization – that is the number of people with Covid-19 in hospital, not the number of people being admitted to hospital – is falling in all states and territories except for Western Australia. Hospitalization by state is shown on the website maintained by Juliette O’Brien and her colleagues. That site also records the number of people in ICU with Covid-19, a more consistent indicator between jurisdictions, as shown in the graph below.
Deaths
Nationally deaths have been falling, at different rates in different states, as shown below.
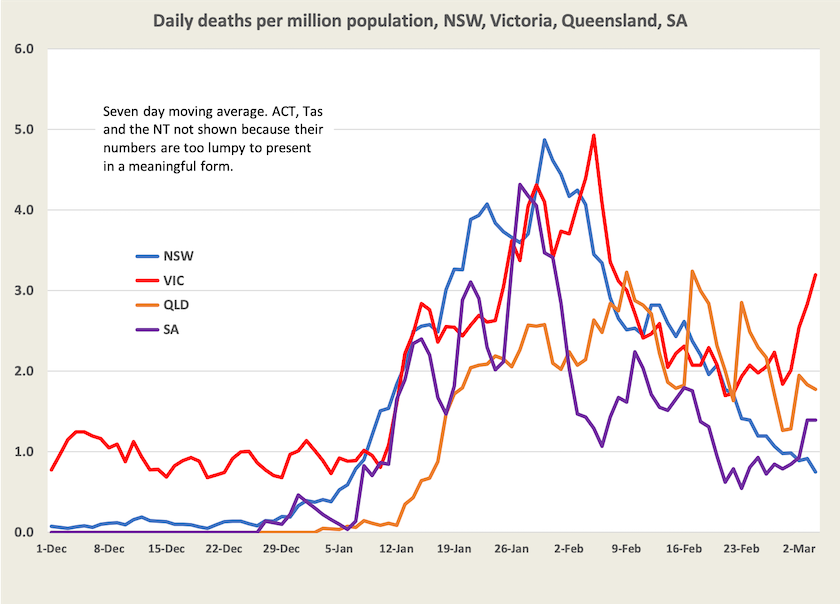
In contrast with other states, where ICU numbers and deaths peaked early and fell sharply, deaths in Queensland have been erratic, without peaking. This possibly reflects the spread of its population. The recent sharp rise in Victorian deaths is notable.
After getting through the first 18 months of the pandemic, up to the end of August last year, Australia had only 1000 deaths from Covid-19. Subsequently there have been another 4200 deaths, 3000 of them in the first two months of this year. Western Australia is yet to experience any significant number of deaths (11 at last count): there will be deaths in that state, but proportionately much lower than in the other states.
For New South Wales and Victoria death rates per case are shown in the graph below, i.e.. the death rate per case recorded three weeks earlier. Notably the death rate in Victoria, having been line with the death rate in New South Wales, is now much higher.
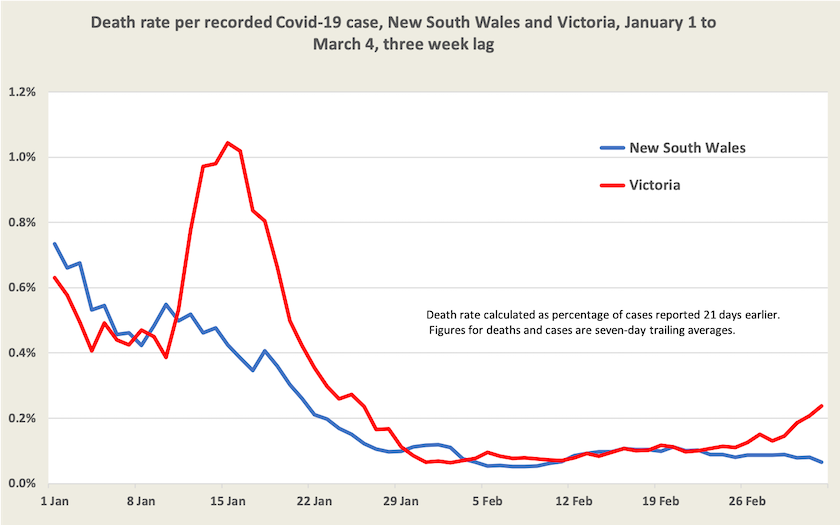
This calculation reveals a death rate per case in New South Wales of about 0.066 percent, or 1 in 1500 cases. (Victoria’s is 0.237 percent, or 1 in 420 cases).
The New South Wales weekly surveillance report to 5 February, shows that of 879 000 cases recorded from November 26 to 5 February there were 938 deaths – a rate of 0.11 percent. This would be consistent with the present rate of 0.08 percent.
The same report reveals that the more infectious (but not more deadly) BA.2 sub-variant of Omicron has been detected in New South Wales.
Vaccination
It’s informative to look at Australia’s vaccine progress, particularly our uptake of a third dose, on the ABC’s vaccine tracker. We did well in achieving a reasonable level of two-dose vaccination, but we have achieved only a 45 percent level of third-dose cover, and the rate of third vaccination has fallen away sharply in the first two months of this year. A bit of back-of-the-envelope arithmetic (75 000 doses a day, 8 million adults still to receive a third dose) suggests it will take another 3 months to get a reasonable level of cover. High-income “developed” European and Asian countries, with which we normally compare ourselves, have third-dose vaccination levels between 50 and 70 percent.
Where to from here? How the pandemic ends: it doesn’t really
The ABC’s Jeremy Fernandez, with input from Hassan Vally of Deakin University and Lara Herrero from Griffith University, has a neat 16-minute presentation How and when will the COVID pandemic end?.
Fernandez explains how different diseases develop, how public health authorities deal with them, how our bodies learn to deal with viruses, and the basic mathematics of disease reproduction (the meaning of “R”).
Covid-19 won’t be eradicated, but it will probably slowly morph from “pandemic” to “endemic”, just as past pandemics, such as the 1918 “Spanish” flu have done. Its path depends on three unknowns – how long vaccines last, how the virus evolves, and how well we treat it. Treatments may be the most effective way to deal with Covid-19 in the future, and there are some highly effective treatments coming along.